What is Mental Health Billing? Complete Guide
The CMS-1500 form is used for single practitioner claims and to submit charges through Medicare Part-B. For mental health providers, the billing process can be challenging but not impossible. If you dig into the points mentioned in this article, you will get where you want to be – having your practice receive the deserving reimbursements on time. A lot of time, mental healthcare professionals find it difficult to juggle between rendering patient care and filing claims. Mental healing requires a lot of collaboration between the medical professional and the patient.
- Partial or incomplete coordination of care will have adverse impacts and will only bring in several inconveniences and discrepancies for both practice and patients.
- Therefore, it is important for everyone to understand what mental healthcare billing is right from its basics.
- By following these insights, you’ll traverse the landscape of mental health billing with confidence, ensuring that financial procedures align seamlessly with the quality of care extended.
- Both undercoding and upcoding are strictly illegal as they do not accurately represent the services rendered and could be construed as fraud by the payers.
- After completing the patient’s assessment test, a psychiatric diagnosis review occurs.
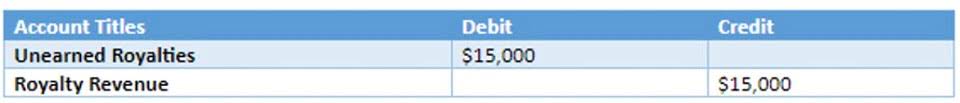
Chapter 5: Refiling Claims, Appeals, Rejections
People become mental health professionals because they want to help others. However, providers cannot help others unless they collect sufficient funds to run their practices, and pay themselves. Some providers will even try to do the billing https://www.bookstime.com/ themselves but eventually this will become overwhelming and create time management problems, not to mention lost income. Mastering mental health billing is pivotal for seamless access to quality care while maintaining financial equilibrium.
- Both medical and mental health billing require the use of ICD-10 and CPT codes.
- In this guide, you’ll learn about the behavioral health modifiers you need to use for billing your insurance claims.
- We cannot and will not advice you to use a single diagnosis code, even though it is a very common practice for therapists to use one code for all of their patients (e.g. anxiety or depression).
- If your questions are not resolved with the above techniques, you can pull the required insurance data from EHR (Electronic Health Record).
- The UB-04 and other mental health forms are uploaded on some compliant software programs, making it easier for you to electronically fill out and file the form.
- In fact, it is important to endorse double-checking in the billing process.
Mental Health Billing for Dummies: The Short Guide

Use your reference ID from your eligibility and benefits verification phone call to fight your case. Once claims are verified as received, it’s time to hurry up and wait until payment. Often processing takes two to three weeks after receipt mental health billing for dummies of the claims, plus the time to mail checks. We cannot and will not advice you to use a single diagnosis code, even though it is a very common practice for therapists to use one code for all of their patients (e.g. anxiety or depression).
Denial Management
ICANotes is the premier EHR for behavioral health specialty, and we work with all clinical disciplines to deliver an intuitive charting solution for your practice. Another tip for submitting claims properly is to familiarize yourself with common claims forms that many insurance companies use, such as the UB-04 form. This form is usually reserved for mental health clinics and specialized health centers for medical billing. The UB-04 and other mental health forms are uploaded on some compliant software programs, making it easier for you to electronically fill out and file the form.
- However, billing for mental health services can often hinder the treatment process if there are coding errors, inaccurate or inefficient documentation and pre-authorization issues.
- If any documentation and pre-authorization is found incomplete or inaccurate, it can cause hindrances in medical billing.
- To avoid the worst results from critical mental health issues, it is crucial to provide therapy as soon as possible.
- Although this sounds like a huge job, in the long run, making sure you know the coverage available for each patient before they receive any services will be very beneficial in the long run.
Familiarity with Mental Health EHRS
Mental health CPT code modifiers can describe the way services are rendered as well, telehealth modifiers as an example. Thank you for substantially helping with this difficult aspect of my practice. I appreciate all your help and the patients are grateful for your courtesy… When considering whether to join a network or accept payment from insurers, it’s important to evaluate their pre-approval rules and their limits for payment.
After all, billing is closer to business administration and finance than it is to healthcare disciplines. To empower mental health professionals in their billing endeavors, we’ll provide a curated list of online resources, tools, and software designed to streamline the billing process. Additionally, recommendations for continuing education in billing practices will be highlighted. In essence, while mental health billing and behavioral health billing share similarities, the latter encompasses a broader array of psychological services. Understanding their relationship is vital for practitioners, insurers, and policymakers working to improve access to comprehensive mental and emotional well-being care. You use this tool every day, so why not make it a habit to check the “claim status” section that’s included with and provided by your clearinghouse?
- This procedure can prolong insurance billing and prevent a patient from receiving the treatment they need.
- When these payers present themselves, it’s not the end of the world but it does present a process change.
- To avoid these situations, it’s a good idea to evaluate clients’ insurance coverage before each visit, if possible.
- Before you “officially” send your claims to your client’s payers your clearinghouse should help you out via scrubbing and rejections.
Well, as I alluded to earlier, the claims that come from hospital visits differ from those in the behavioral health world. After all, there are differences between the types of claims that hospitals submit compared to those coming from mental health facilities. Although the billing rules within the mental health space seem archaic, the practice sends shivers down the spine across the entire medical world…regardless of specialty. Using the wrong CPT code could result in a significant impact on the claims submission process. Therefore it is important to make sure that no mistake is made even accidentally. A VOB can assist in eliminating denied claims and unpaid bills for the services that are rendered to the patient.
The billing process, from scheduling an appointment to reimbursement, requires careful attention to detail to ensure accuracy and compliance. Mental health billing stands as a pivotal mechanism to guarantee individuals’ access to vital mental health services and treatments. This process entails intricate procedures, coding precision, and meticulous documentation, all aimed at facilitating reimbursements from insurance providers.